The Challenge
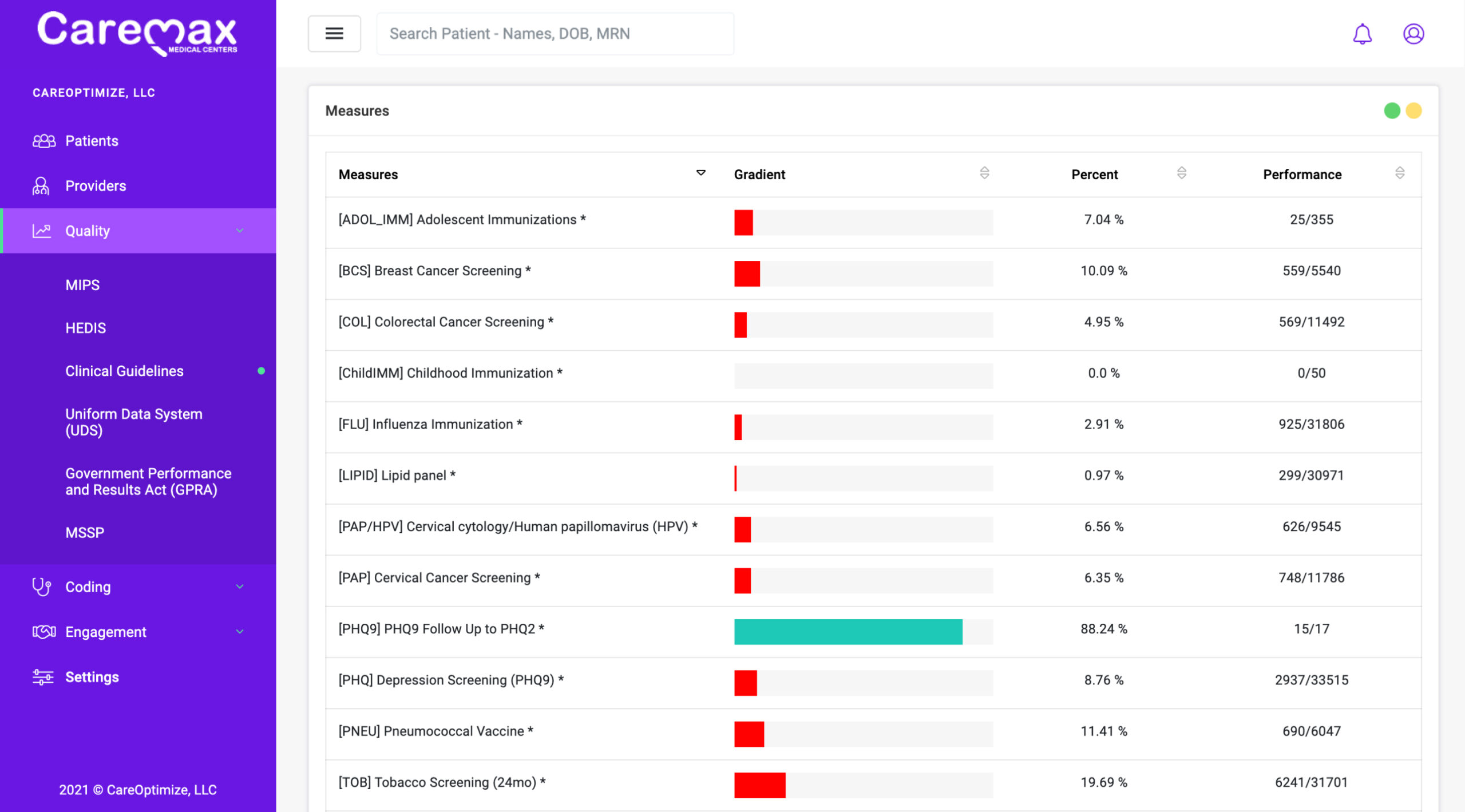
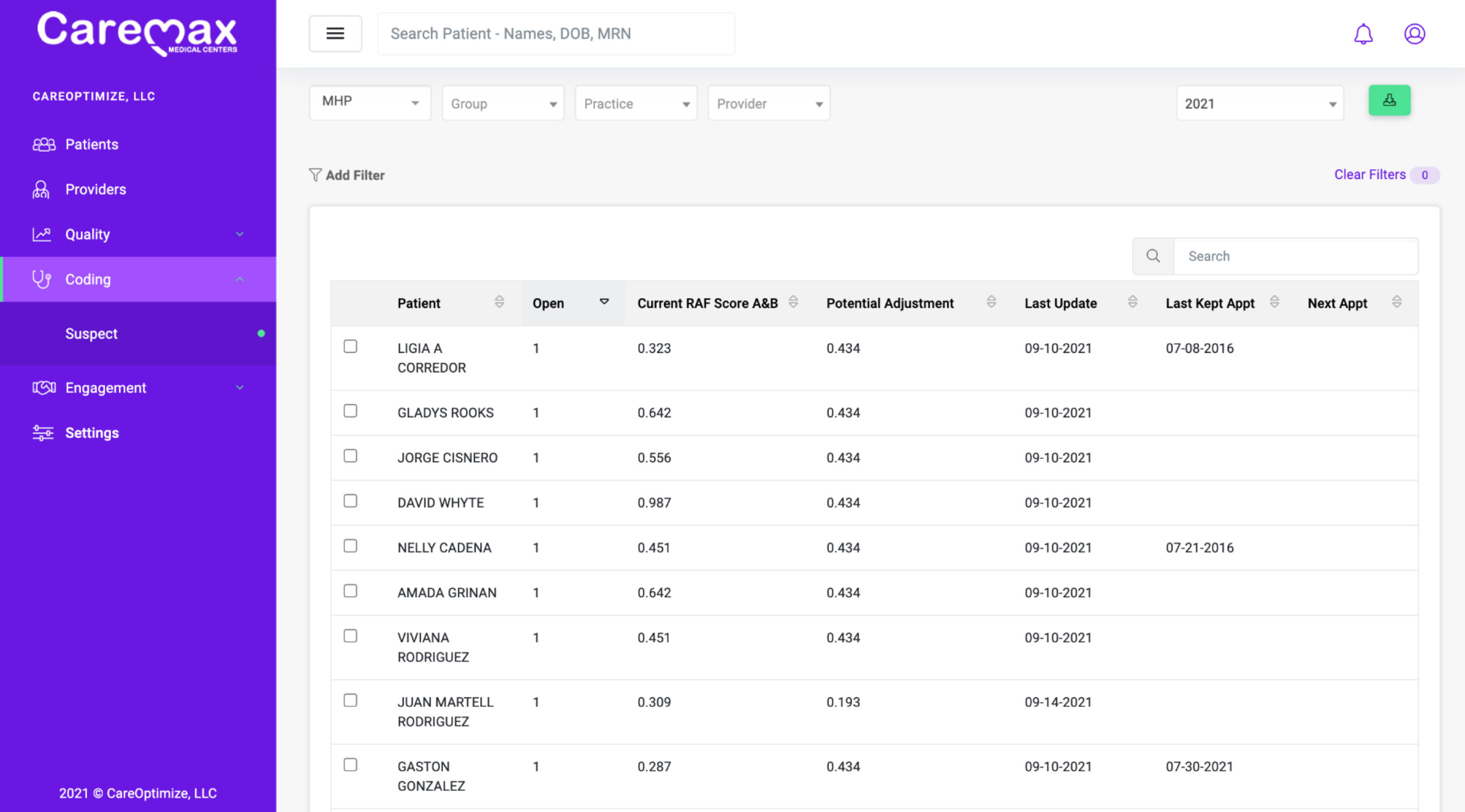
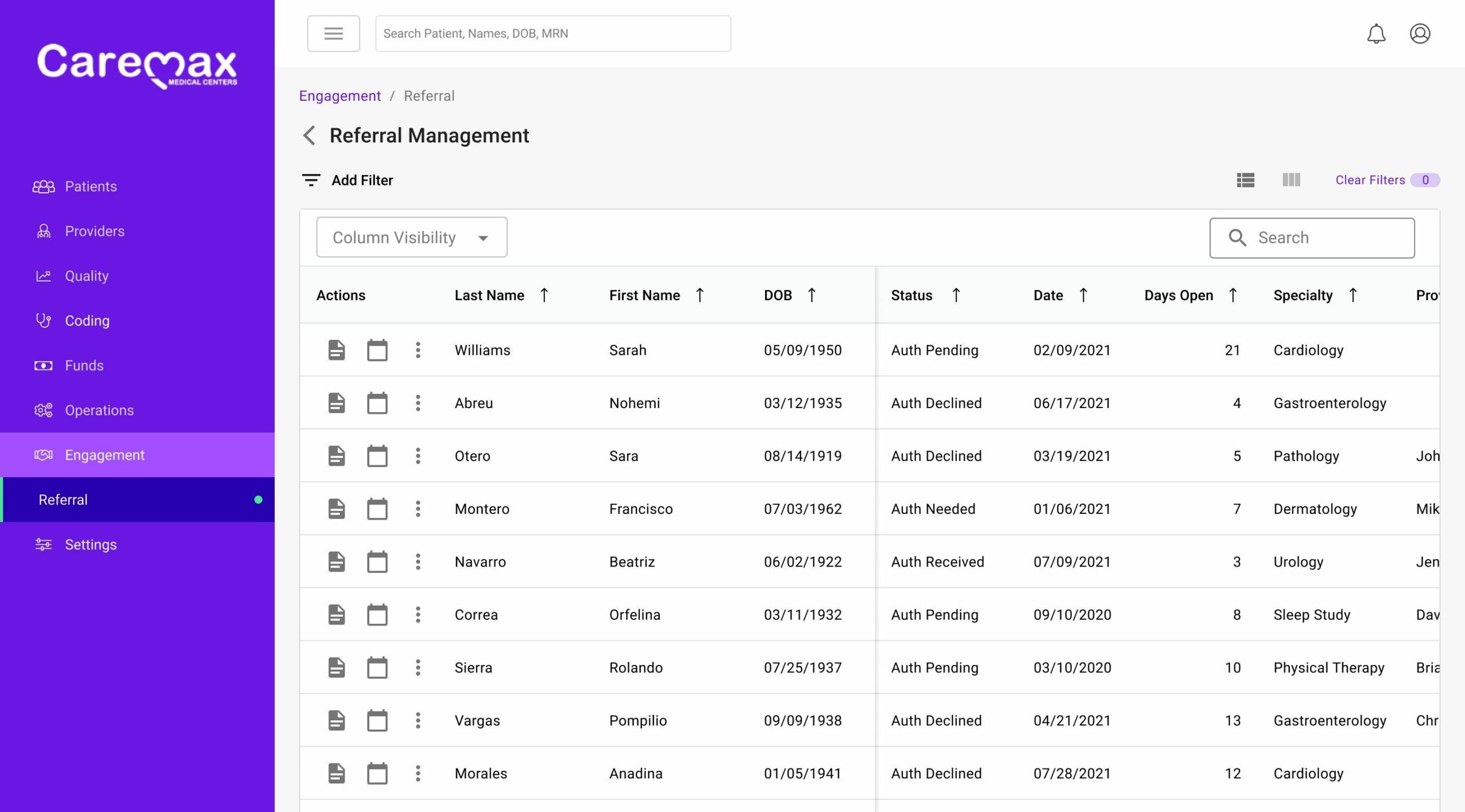
Fragmented systems create additional challenges for providers participating in risk adjusted programs. Payer initiatives are displayed through portals that are removed from the current workflow. Retrospective chart audits by coders often take months to complete. Having to consider each initiative is a distraction for providers that need to be focused on offering patients the best care.
To make matters worse, revenue is tied to how well each provider scores on each initiative. If performance metrics slip, then compensation is reduced.

CareOptimize
simplify workflows with intelligent solutions
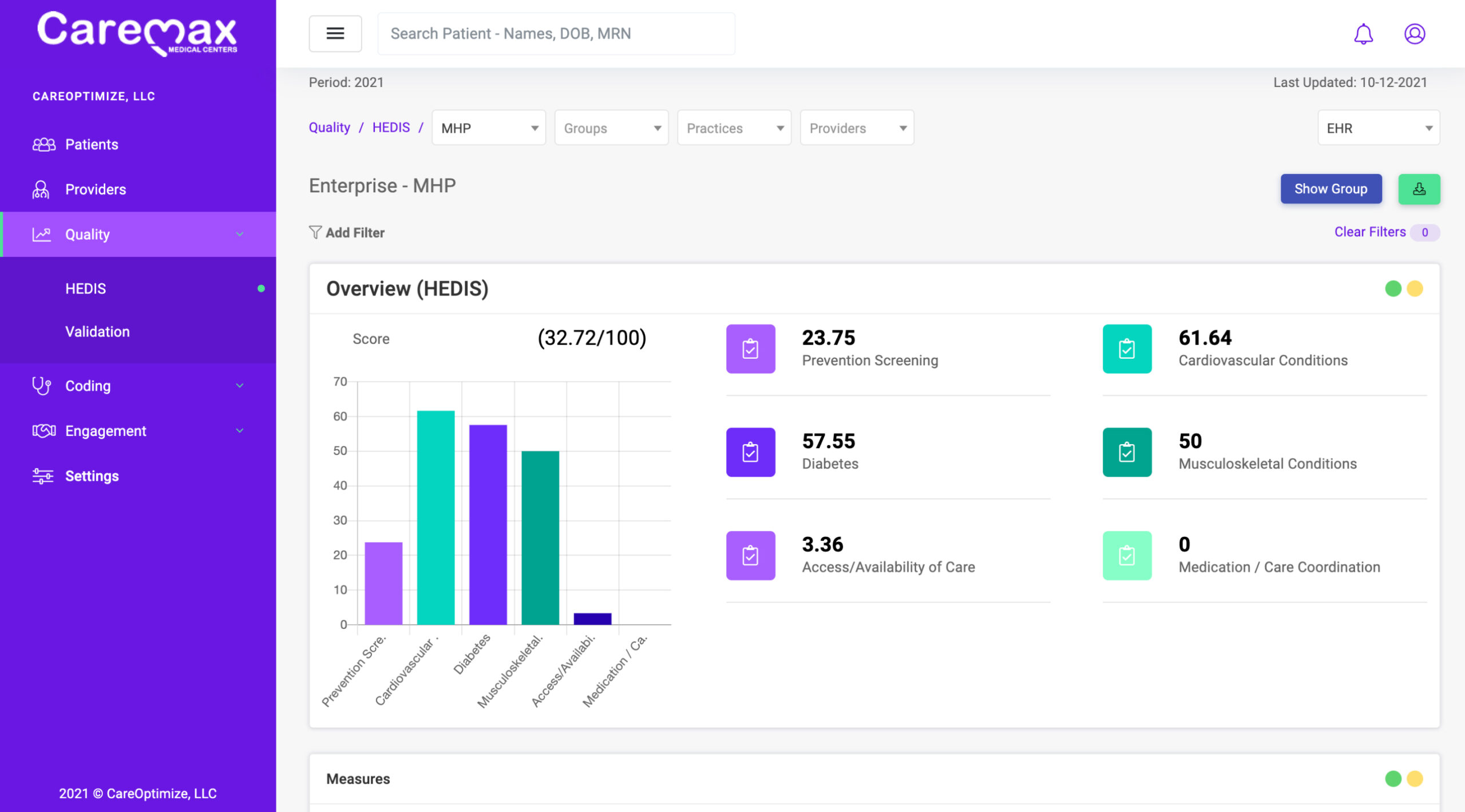
CareOptimize combines clinical data and health plan quality performance metrics to cultivate autonomous documentation suggestions. Powered by a machine learning rules engine, our solutions are flexible enough to accommodate current practice workflows while simultaneously reducing friction at the point of care. Best of all, tedious quality and coding requirements now become a seamless part of each patient encounter.